What Is Progressive Familial
Intrahepatic Cholestasis (PFIC)?
PFIC is a group of rare, inherited diseases that mostly affects the liver. There are 3 main types of PFIC and several other, rarer types. These are all called subtypes. The 2 most common subtypes are PFIC2 and PFIC3.
The 3 main types of PFIC
How does PFIC affect the liver?
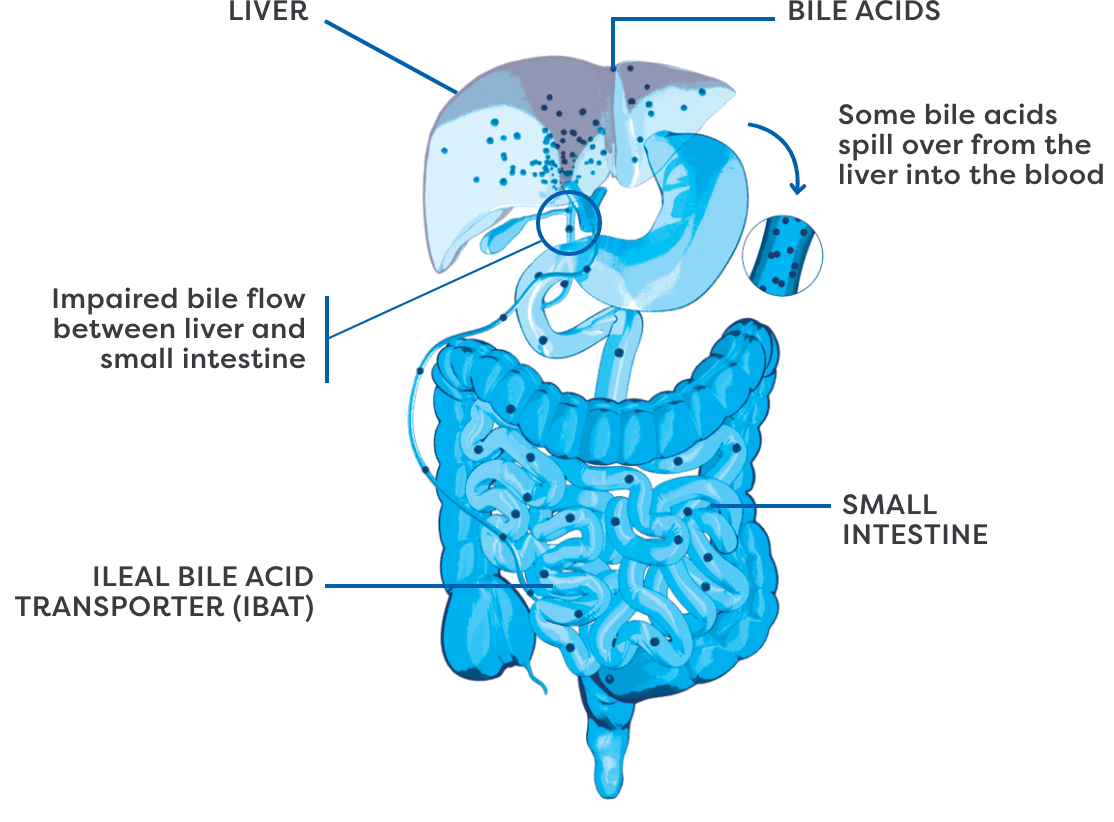
The liver makes a fluid called bile that helps with the digestion of fats. Bile acids, which are a part of bile, are made by the liver cells.
In PFIC, bile acids get stuck inside the cells.
Over time, bile acids build up in the liver and blood.
95% of bile acids made by the liver are recycled in the intestine through the IBAT.
What are the effects of bile acid buildup?
When bile acids build up in the liver, they spill over into the bloodstream. This can cause an increase in bile acids throughout the entire body. These high levels of bile acids are an underlying cause of cholestatic pruritus (itch) in PFIC.
A COMMON AND CHALLENGING SYMPTOM
Cholestatic pruritus affects most people with PFIC (76% to 100%) and is also the most burdensome symptom.
The scratching is a signal
Over time, the buildup of bile acids in the liver can lead to long-term problems, including:

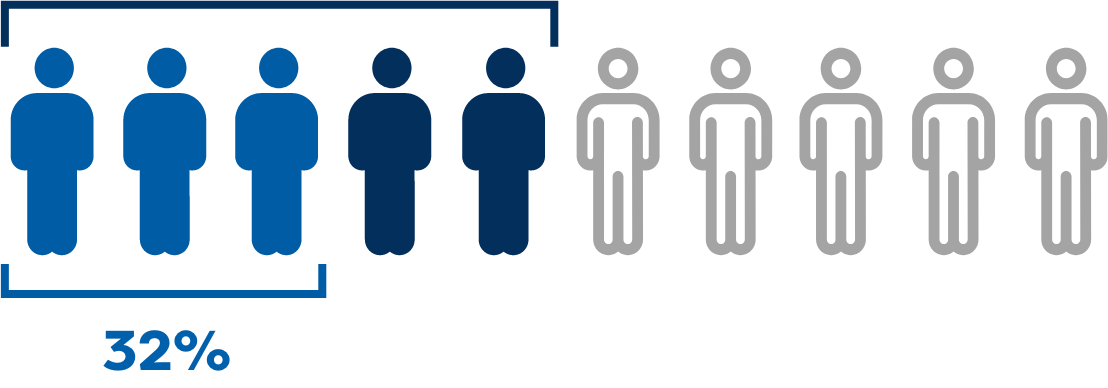
Research has shown that approximately
50%
of patients with PFIC1 or PFIC2 still have their own liver by age 10.
- In PFIC2, specifically, only 32% of patients still have their own liver by age 18


Cholestatic pruritus is more than just scratching
Cholestatic pruritus is often a very challenging symptom for people with PFIC.
Cholestatic pruritus is frequently first seen by age 3 months in people with PFIC1 and PFIC2 and by age 2 years to 3 years in people with PFIC3.
Beyond the scratching, it can be difficult to navigate all aspects of cholestatic pruritus without the right support. Signs and symptoms related to cholestatic pruritus can look different during the day and/or night and vary for each person.
The burden of cholestatic pruritus
Approximately 60% of caregivers report that their child suffers from sleep disturbances due to itch.
Sleep disturbances include needing help falling asleep, needing soothing, and sleeping with a caregiver.
Additional signs and symptoms related to cholestatic pruritus can include:






ALL LEVELS OF CHOLESTATIC PRURITUS DESERVE ATTENTION
Share your experience with cholestatic pruritus with your doctor and let them know about any changes in symptoms. Not sure where to start? Visit our Resources page before your next doctor’s appointment to help guide the discussion.
What else should you know about cholestatic pruritus in PFIC?
start early
Cholestatic pruritus is frequently first seen by age 3 months in people with PFIC1 and PFIC2 and by age 2 years to 3 years in people with PFIC3.
the surface
Treatment options for cholestatic pruritus in PFIC have been limited. In cases where cholestatic pruritus is unmanageable, many people still choose to have surgery and/or a liver transplant.
is often normalized and overlooked
It can be hard to recognize the impact of cholestatic pruritus on daily life. Symptoms of cholestatic pruritus may start to seem normal or become routine over time, making them easier to downplay or minimize.